A molecular switch for stomach disease
Mechanism which leads to stomach disease triggered by Heliobacter pylori decoded
Infectious diseases triggered by bacteria and other microbes are the most frequent cause of human mortality across the globe. Roughly half of the world’s population carry the bacteria Helicobacter pylori (H. Pylori) in their stomach, known to be the most significant risk factor for ulcers, MALT lymphoma and adenocarcinoma in the stomach. The rapid spread of pathogens resistant to medication such as antibiotics is making it increasingly difficult to treat infections such as these using antimicrobial therapies. A research team from FAU has now revealed a new mechanism which controls the causes of infection with H. pylori, triggering the development of stomach diseases. It is hoped that these findings will lead in time to new therapies. The study was published in the journal Nature Communications.
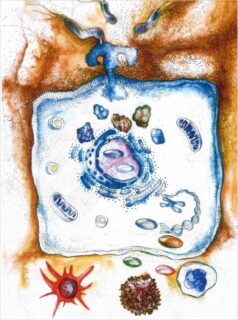
A team of national and international scientists led by Prof. Dr. Steffen Backert from the Chair of Microbiology at FAU has investigated how the bacteria manipulate the host’s immune system in order to ensure their long-term survival in the stomach. A chronic inflammation is the most common cause for stomach illnesses such as these. The researchers have identified a ‘molecular switch’ which uses a previously unknown mechanism to regulate the inflammation reaction in the stomach. The interaction between H. pylori and stomach cells activates a syringe-like pilus structure referred to as a type IV secretion system. A protein, CagL, is presented at the surface of this structure which allows the bacterial toxin known as CagA protein to be delivered into the stomach cells. The injected CagA then re-programmes the host cell so that stomach cancer can develop. It now appears that CagL also has another important function, however. The protein is recognised by the immune system via the receptor TLR5. Experiments in mouse models have demonstrated that TLR5 controls the infection efficiently. CagL imitates a TLR5 recognition motif in the flagellin protein of other pathogens, thereby controlling the human immune response.
Interestingly, this signalling pathway can be both switched on and switched off by the type IV secretion system, which is not thought to be the case with other bacteria. Presumably, H. pylori has exploited this signalling pathway over thousands of years of evolution to eliminate ‘bothersome’ bacterial competitors in the stomach. At the same time, CagL influences the congenital and adaptive immune system as well as the inflammation reaction in such a way that H. pylori itself is not recognised and therefore cannot be eliminated – a mechanism which is crucial for long-term infections with H. pylori in the stomach and triggering stomach disease. Researchers also observed that TLR5 is no longer produced in healthy stomach cells and once an infection has been resolved. This indicates that the expression of this protein is a new indicator for stomach disease in humans triggered by H. pylori.
New approach for treating stomach disease
Prof. Backert hopes that these findings will help develop significant new approaches for anti-bacterial treatment, as CagL, CagA and TLR5 lend themselves well to treatment. The participating researchers have already started to test appropriate substances. ‘We hope that specific inhibitors can paralyse the function of the type IV secretion system, or partially or entirely prevent infection,’ reports Prof. Backert.
The publication is the result of many years of research at the Chair of Microbiology at FAU funded by the German Research Foundation as part of Collaborative Research Centre (SFB) 1181 ‘Schaltstellen zur Auflösung von Entzündung’ (switching points for resolving inflammation) and carried out in collaboration with other working groups from Germany, Switzerland, Korea and India.
Further information
Prof. Dr. Steffen Backert
Phone: + 49 9131 28081
steffen.backert@fau.de